Psilocybin and Antidepressants: Drug Interaction
Introduction
Psilocybin, a naturally occurring psychedelic compound found in certain species of mushrooms, has garnered significant attention for its potential therapeutic benefits in treating mental health conditions, including major depressive disorder (MDD). Recent clinical trials have shown promising results in using psilocybin-assisted therapy to address treatment-resistant depression (TRD). Unlike traditional antidepressant drugs, which often require chronic administration and can lead to antidepressant drug withdrawal, psilocybin offers a novel approach with its profound and rapid effects on mood and perception. However, the interaction between psilocybin and antidepressant medications, particularly selective serotonin reuptake inhibitors (SSRIs), remains an area of active research. This article aims to provide an overview of the current state of research on psilocybin therapy for MDD, including its efficacy, safety, and potential interactions with antidepressant medications.
Psilocybin and antidepressants
At Essence, we are committed to empowering our visitors with reliable information and valuable insights into the realm of psychedelic research and mental health treatments. A crucial topic we address is the interplay between psilocybin and antidepressants. Our goal with this content is to provide education and awareness, enabling you to grasp the possible risks and nuances in this field. Please read on to learn more about this vital subject.
Antidepressants
Antidepressants are a broad category of medications used primarily to treat depression. They can also be effective in treating a range of other conditions, including anxiety and chronic pain management. These drugs work by altering the chemicals in the brain responsible for mood and emotional states.
Antidepressants operate by influencing the brain’s chemical messengers, primarily neurotransmitters like serotonin, norepinephrine, and dopamine.
For instance, Selective Serotonin Reuptake Inhibitors (SSRIs) are a class of antidepressants that work by blocking the reuptake of serotonin in the brain, making more serotonin available to improve transmission of messages between neurons.
Another type, Tricyclic Antidepressants (TCAs), increase the levels of norepinephrine and serotonin, and block the action of acetylcholine, which helps to balance mood and alleviate depressive symptoms. Meanwhile, Monoamine Oxidase Inhibitors (MAOIs) inhibit the activity of monoamine oxidase, an enzyme that breaks down serotonin and norepinephrine, thus increasing their levels in the brain and improving mood and emotional balance.
Each of these mechanisms targets the complex neurochemical pathways involved in mood regulation, aiming to correct imbalances that contribute to depressive states.
Psilocybin
Psilocybin is a naturally occurring psychedelic compound produced by certain species of mushrooms, often referred to as “magic mushrooms”. This substance has been the subject of increasing scientific study due to its potential to significantly impact mental health conditions, including depression (or treatment-resistant depression) and anxiety.
Unlike antidepressants, which are taken regularly and work by adjusting brain chemistry over time, psilocybin offers a different approach. Psilocybin mushroom effects during and after the experience produce profound changes in consciousness and perception, often described as acute subjective psychedelic effects, which can lead to rapid and lasting changes in mood and outlook. Psilocybin has shown promise for treatment-resistant depression or major depression as well.
Psilocybin’s chemical composition is intriguing, with its molecular formula being C12H17N2O4P. This compound is a tryptamine alkaloid, structurally similar to the neurotransmitter serotonin and its interaction with serotonin receptors - especially 5-HT2A - plays a key role in its effects on mood regulation, anxiety, and emotional processing. Please read more about psilocybin use in depression treatment in “Single-Dose Psilocybin Treatment for Major Depressive Disorder – A Randomized Clinical Trial”.
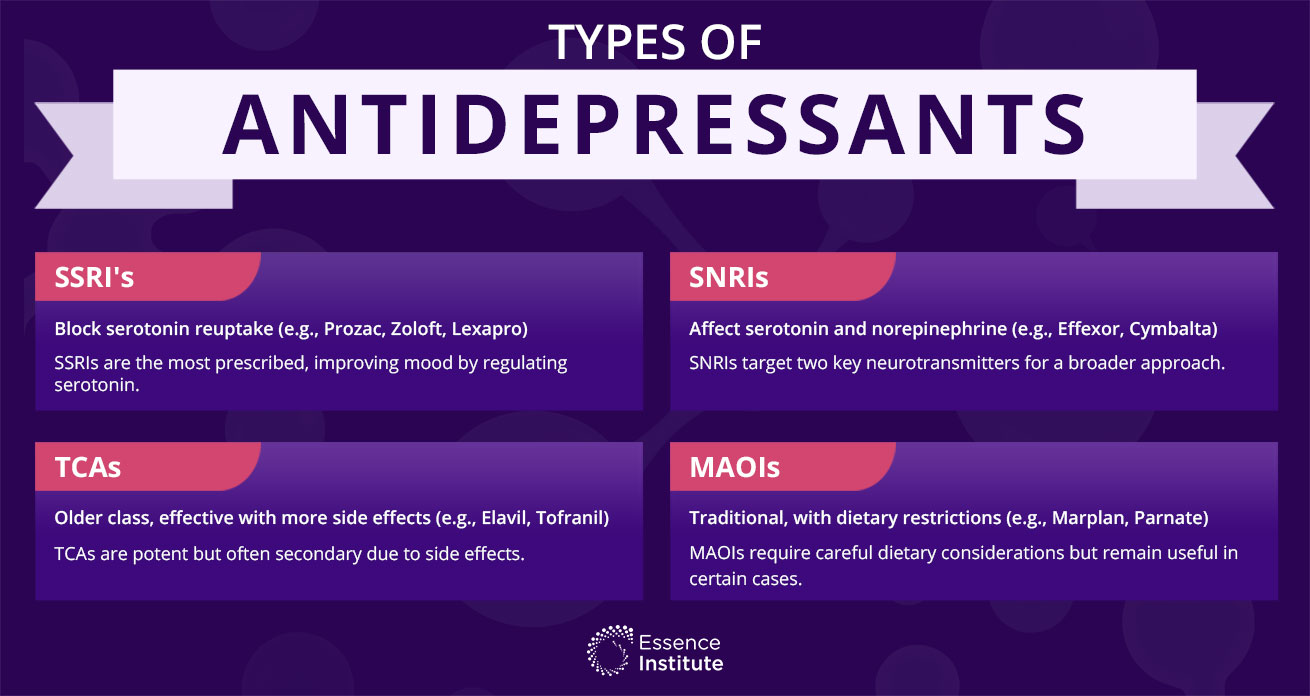
Types of Antidepressants
Antidepressants come in several forms, most commonly SSRIs (Selective Serotonergic Reuptake Inhibitors), SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors), and MAOIs (Monoamine Oxidase Inhibitors) etc.
SSRI’s
Selective serotonin reuptake inhibitors (SSRI's) are the most commonly prescribed antidepressants. They work by blocking the reuptake of serotonin, a neurotransmitter that helps regulate mood and emotional states. SSRIs include drugs like Prozac, Zoloft, Celexa, Paxil and Lexapro.
Specific variants are (generic name, brand name(s)):
Serotonin Norepinephrine Reuptake Inhibitors (SNRI's)
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) offer another avenue for treating depression by simultaneously affecting two critical neurotransmitters in the brain. This class of medication includes drugs like Effexor, Pristiq, Cymbalta and Savella.
Specific variants are (generic name, brand name(s)):
Tricyclic Antidepressants (TCA’s)
Tricyclic Antidepressants (TCAs) represent an older class of antidepressants that, despite the advent of newer medications, remain a critical option for certain patients due to their unique mechanism of action and effectiveness. Due to more side-effects they are mostly not the first choice.
Specific variants are (generic name, brand name(s)):
Monoamine-oxidase inhibitors (MAOI’s)
Monoamine-oxidase inhibitors (MAOI's) represent a traditional category of antidepressants, particularly the earlier versions. They exhibited a higher incidence of side effects, with some posing risks when consumed alongside tyramine-containing foods such as certain cheeses and sauerkraut.
Specific variants are (generic name, brand name(s)):
Psilocybin Therapy for Major Depressive Disorder
Psilocybin therapy has shown remarkable efficacy in reducing symptoms of depression in patients with treatment-resistant depression (TRD). A recent study published in the Journal of Psychopharmacology found that psilocybin-assisted therapy led to significant improvements in depressive symptoms, with 67% of participants achieving remission at three weeks post-treatment. This rapid and sustained response contrasts with the gradual effects typically seen with traditional antidepressant drugs. Another study published in the Journal of Clinical Psychopharmacology reported that psilocybin therapy not only reduced depressive symptoms but also enhanced the overall quality of life for patients with major depressive disorder (MDD). These findings underscore the potential of psilocybin-assisted therapy as a transformative treatment for those who have not responded to conventional antidepressant treatments.
Psilocybin and antidepressants
The intersection of psilocybin and antidepressants in mental health treatment marks a fascinating frontier in modern psychiatry, inviting a deeper exploration of their potential synergies and differences. While antidepressant drugs prior use can impact the efficacy of psilocybin treatment, antidepressants work by altering brain chemistry over time, whereas psilocybin can induce a powerful and immediate change in perception during the experience. Let’s delve into the interaction between Psilocybin and Antidepressants by taking a closer look.
How Does Psilocybin Work?
Psilocybin interacts with the brain in a fascinating and complex way, primarily affecting the serotonin 2A receptor (5-HT2A). This receptor is responsible for regulating the flow of information between neurons, and its activation by psilocybin leads to changes in brain activity that give rise to altered states of consciousness. The effects of psilocybin can include enhanced introspection, increased emotional openness, and a sense of connection with others and the world around us.
Upon ingestion, psilocybin is quickly metabolized into psilocin, which then exerts its psychoactive effects by binding to serotonin receptors in the brain, particularly the 5-HT2A receptor. This interaction is thought to produce the profound changes in perception, mood, and thought associated with psilocybin use.
While the psychedelic experience is the intended outcome of psilocybin, there is much more to it. Extensive research has been conducted on the safety of psilocybin (as well as other psychedelics). The findings are promising: psilocybin exhibits low toxicity and does not result in organ damage or neuropsychological deficits.
During the course of the experience, certain physiological symptoms may manifest, including dizziness, weakness, tremors, nausea, drowsiness, paresthesia, blurred vision, dilated pupils, and heightened tendon reflexes.
How Antidepressants work?
We have already explored this topic above while introducing different types of Antidepressants in this article above. In summary, antidepressants work by altering levels of neurotransmitters in the brain, particularly serotonin. This can help balance moods and emotions, alleviating symptoms of depression and anxiety.
Antidepressant Use and Psilocybin Therapy
The use of antidepressant medications, particularly selective serotonin reuptake inhibitors (SSRIs), is widespread among patients with major depressive disorder (MDD). However, the interaction between psilocybin and SSRIs is not fully understood. Some studies suggest that SSRIs may attenuate the effects of psilocybin, potentially diminishing its therapeutic impact.
Conversely, other research has found no significant interaction between SSRIs and the acute subjective effects of psilocybin. For instance, a recent study published in the Journal of Psychopharmacology indicated that SSRIs did not significantly alter the acute subjective psychedelic experience of psilocybin in patients with TRD.
Despite these mixed findings, it is clear that further research is needed to fully elucidate the interaction between psilocybin and antidepressant medications, ensuring safe and effective treatment protocols.
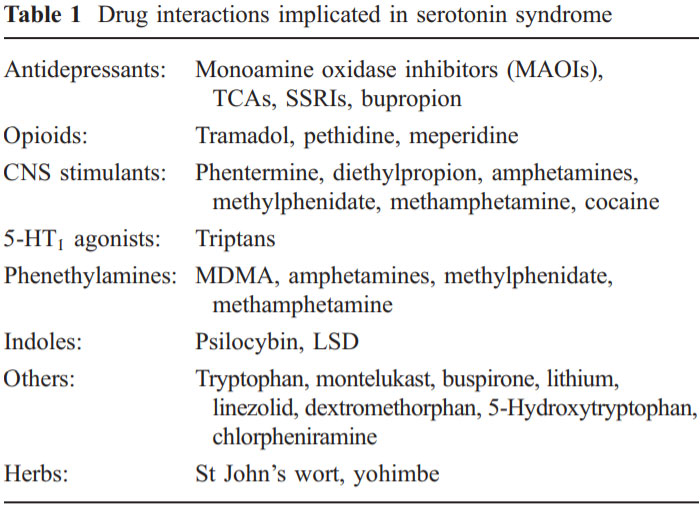
Drug Interaction
The interaction between psilocybin and antidepressants is not fully understood, but it involves the shared pathway of serotonin regulation. When combined, these substances may alter the effects of one another in unpredictable ways. Since this topic is still a relatively new area of research, there were no reports or clear guidelines on the potential risks and benefits of combining psilocybin with antidepressants.
Serotonin Syndrome
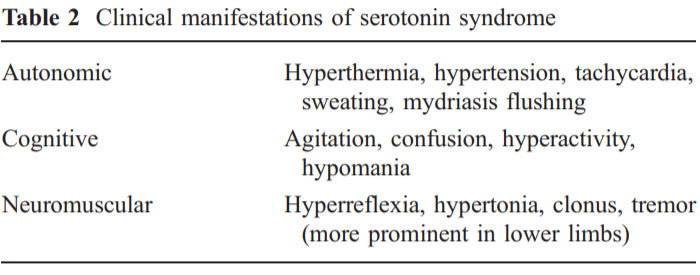
Serotonin Syndrome is a potentially serious condition that can occur when levels of serotonin become too high, often as a result of interaction between medications that affect serotonin metabolism.
Symptoms include confusion, agitation, rapid heart rate, dilated pupils, muscle rigidity, elevated heart rate and blood pressure, seizures and in severe cases, it can be life-threatening.
The interaction between psilocybin and antidepressants is not fully understood, but it involves the shared pathway of serotonin regulation. When combined, these substances may alter the effects of one another in unpredictable ways. Since this topic is still a relatively new area of research, there were no reports or clear guidelines on the potential risks and benefits of combining psilocybin with antidepressants.
While rare, the combination of psilocybin and SSRI SNRI antidepressant use may increase the risk of serotonin syndrome. Therefore, it is crucial for individuals using both substances to consult with your GP or psychiatrist before going on a retreat. They can (possibly) help you to discontinue the antidepressants before going on a retreat.
Attenuation of psilocybin mushroom (Decreased Effectiveness)
Effects of psilocybin combining with antidepressants can have the possibility of reduced drug effects. When considering psilocybin therapy versus escitalopram, some studies have suggested that certain antidepressants may interfere with the psychedelic experience, potentially dulling its effects. This could have implications for the therapeutic potential of psilocybin, as it may diminish any positive impact on mental health conditions such as depression and anxiety
Prolonged Effects
Some antidepressants, particularly MAOIs, can inhibit the breakdown of psilocybin and prolong its effects. This could lead to longer-lasting psychedelic experiences, which may not be desirable for all individuals. It is therefore essential to discuss any ongoing medication use with a healthcare provider before embarking on a psilocybin journey.
Clinical Trials and Research
Several clinical trials are currently underway to investigate the efficacy and safety of psilocybin-assisted therapy for major depressive disorder (MDD). The COMP360 trial, a phase II clinical trial, is one such study exploring the safety and efficacy of psilocybin-assisted therapy in patients with treatment-resistant depression (TRD). Preliminary results from this trial have been promising, showing significant reductions in depressive symptoms and improvements in quality of life. Additionally, the Psilocybin-Assisted Therapy for Depression (PAT-D) trial is another key study examining the potential benefits of psilocybin therapy for MDD. These trials contribute to a growing body of evidence supporting the use of psilocybin-assisted therapy as a viable treatment option for depression, particularly for those who have not found relief with traditional antidepressant drugs.
Safety and Efficacy Considerations
Psilocybin-assisted therapy has generally been shown to be safe and well-tolerated in patients with major depressive disorder (MDD). However, potential risks and side effects include anxiety, agitation, and, in rare cases, psychosis. It is crucial to note that psilocybin therapy is not recommended for individuals with a history of psychosis or major comorbid psychiatric disorders. Additionally, the use of psilocybin in patients taking antidepressant medications, particularly selective serotonin reuptake inhibitors (SSRIs), requires careful consideration and monitoring. The interaction between these substances can be complex, and further research is needed to fully understand their combined effects. Ensuring the safety and efficacy of psilocybin-assisted therapy involves a comprehensive approach, including professional supervision, gradual discontinuation of antidepressants if necessary, and close monitoring for any adverse effects.
Recommendations
In light of the complex interactions between psilocybin and antidepressants, navigating their combined use requires careful consideration and guidance from healthcare professionals.
FAQ
Consult with a healthcare provider as combining these two can lead to serious health risks.
Seek immediate medical attention if you suspect Serotonin Syndrome.
Yes, under the guidance of professionals and in legal settings.
References
For further reading and scientific research on the topic, please refer to the provided references or reach out to us. Our commitment is to bring well-researched, accurate information within your reach, fostering safe and informed choices in the landscapes of mental health and psychedelic therapy.
- 1Carhart-Harris, R. L. (2019). How do psychedelics work? Current Opinion in Psychiatry, 32, 16-21. doi:10.1097/yco.0000000000000467
- 2Johnson, M., Richards, W., & Griffiths, R. (2008). Human hallucinogen research: guidelines for safety. Journal of Psychopharmacology, 22(6), 603–620. doi:10.1177/0269881108093587
- 3Griffiths, R. R., Richards, W. A., McCann, U., & Jesse, R. (2006). Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology, 187(3), 268–283. doi:10.1007/s00213-006-0457-5
- 4Halpern, J. (2003). Hallucinogen persisting perception disorder: what do we know after 50 years? Drug and Alcohol Dependence, 69(2), 109–119. doi:10.1016/s0376-8716(02)00306-x
- 5Dos Santos, R. G., Bouso, J. C., Alcázar-Córcoles, M. Á., & Hallak, J. E. C. (2018). Efficacy, tolerability, and safety of serotonergic psychedelics for the management of mood, anxiety and substance use disorders: a systematic review of systematic reviews. Expert Review of Clinical Pharmacology 11(9), 889 – 902. doi:10.1080/17512433.2018.1511424
- 6Erritzoe, D., Roseman, L., Nour, M. M., MacLean, K., Kaelen, M., Nutt, D. J., & Carhart-Harris, R. L. (2018). Effects of psilocybin therapy on personality structure. Acta Psychiatrica Scandinavica. doi:10.1111/acps.12904
- 7Arora, B., & Kannikeswaran, N. (2010). The serotonin syndrome—the need for physician’s awareness. International Journal of Emergency Medicine, 3(4), 373–377. doi:10.1007/s12245-010-0195-7Drug Interaction
- 8https://jamanetwork.com/journals/jama/fullarticle/2808950